Root Canal Treatment
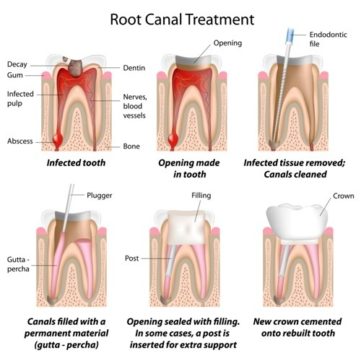
Endodontics is more commonly known as Root Canal Treatment. Such treatment is carried out when the pulp (soft tissue inside a tooth) is either inflamed or dead. The pulp is a tissue made up of nerves, connective tissue and blood vessels.
The pulp may become inflamed or may die if either there is significant decay in a tooth, if there is a large restoration (filling or crown) or if the tooth has been subjected to trauma.
The inflamed pulp may cause toothache or remain pain-free. When the pulp dies, the space it inhabits (the root canal) rapidly becomes infected with bacteria. This may cause pain and swelling in the supporting tissues (abscess) or the tooth may remain symptom-free.
The purpose of root canal treatment is to remove the inflamed tissue or bacteria inside the root canal and thus allow the surrounding tissues to heal.
After cleaning the root canal system, the space created is filled with a root filling to prevent reinfection. A material called gutta percha is used as the root filling material. This a natural substance very similar to rubber
The root canal system, especially in molars, is often complex and difficult to clean well. This is why many general dentists prefer to refer these cases to a specialist who has the training, equipment and experience to deal with them well. The treatment can be time consuming due to it’s complex nature.
A consultation is required to assess what treatment is needed for each individual patient, and a bespoke treatment cost will be presented after the initial appointment.
Please contact us to arrange an appointment.
Frequently asked questions for endodontic treatment
Endodontic Retreatment
Prices
If a tooth has previously had root canal treatment elsewhere an additional £140 will be added
| Treatment | Price |
|---|---|
| Consultation | £90 |